Bovine digital dermatitis (BDD) was first described in the UK in 1987 (Blowey, 1987) and quickly became the most prevalent infectious foot disease of cattle in the UK in the 1990s (Borgmann et al, 1996) and is endemic worldwide. A recent meta-analysis of UK lameness research reported the incidence rate of BDD at 53.6 cases per 100 cow-years (Afonso et al, 2020). Given that BDD is estimated to cost $132 per case (Cha et al, 2010) and is a serious welfare concern, this is an area where there is opportunity for veterinary surgeons to have a positive impact.
Diagnosis of bovine digital dermatitis
A reliable and affordable diagnostic test for BDD is not available and so the gold standard for diagnosis remains lifting feet for examination in a foot-trimming crush. This is time-consuming and therefore impractical from a labour perspective, but also uses time when cows could be resting or eating. Mobility scoring is often used to identify lame cows, however for BDD, only 39% of cattle with severe lesions are detected as lame (Frankena et al, 2009). Frequently farms rely on identifying lesions during foot-trimming, but this means treatment will be delayed and often lesions will have become chronic before they are identified. Alternative methods for assessing within-herd prevalence and for identifying acute lesions for treatment are therefore required and this needs to be an active process.
Lesions are often classified using the ‘M-scoring’ system (where ‘M’ means ‘Mortellaro’) devised by Döpfer and colleagues and later revised (Döpfer et al, 1997; Berry et al, 2012). There has been some success in M-scoring in the parlour after washing cows’ feet and using a head lamp and mirror to aid inspections (Relun et al, 2011; Solano et al, 2017). Both studies showed good sensitivity and specificity for classifying presence/absence of lesions (90–92% sensitivity, 80–88% specificity), but this was reduced when classifying lesion stages, particularly for M1 and M4.1 (Solano et al, 2017). Missing front foot lesions (approximately 10%) and those on the dorsal surface of the foot (approximately 2%) account for most of the decreased sensitivity compared with the gold standard (Solano et al, 2017). Washing of feet in the parlour does improve sensitivity of lesion detection. A survey in 21 herds comparing the methods showed that a median of 32% more cases were detected after washing. It is recommended to apply milking equipment before washing and to angle the hose downward to minimise splashing of faeces-contaminated water onto the udder and teats (Oliveira et al, 2017). Scoring of youngstock and milking cows walking freely in their housing, or milking cows restrained in headlocks is less sensitive than scoring in the parlour (and approximately 50–60% of those identified in a foot-trimming crush), however may still be suitable for assessing trends of BDD prevalence in a herd, for example following changes to disease control plans (Jacobs et al, 2017; Solano et al, 2017).
The use of serology for diagnosing BDD in individual animals is limited because the disease is endemic and therefore the presence of antibodies does not correlate with presence/absence of lesions. A recent study showed increased levels of IgG1 are correlated with presence of lesions, but indirect enzyme-linked immunosorbent assay (ELISA) still misclassified a substantial number of clinically affected animals as negative (81/204, 39.7%) as absorbance readings were so variable (Afonso et al, 2021). It may be more appropriate to apply these methods to estimate herd-level prevalence for disease monitoring purposes. It has been demonstrated that indirect ELISA using bulk tank milk samples is able to distinguish low (≤10%), medium (10–40%) and high (>40%) prevalence herds with good sensitivity (84–97%) and specificity (86–100%) (Aubineau et al, 2021). If further validated, bulk tank sampling has potential to rival time-consuming BDD prevalence estimates made by other methods.
Progress has also been made using higher-tech solutions for detection of BDD, which have potential to improve animal welfare. Computer vision methods have been used for detection of BDD. A database of images of the interdigital space from cows affected by BDD was used to train a BDD detection model to identify and classify lesions. It was able to correctly identify 70.8% of lesions according to internal validation, and 88.2% according to external validation. M2 lesions were less accurately classified than M4, likely because of fewer images available for model training (Cernek et al, 2020). There is also interest in the use of thermal imaging for detection of BDD. It has been shown that interdigital skin temperature pre-calving has a sensitivity of 77% and specificity of 66% for detecting active BDD lesions (Anagnostopoulos et al, 2021).
Individual treatment
Historically antibiotic footbathing was widely used as a vehicle for treatment of BDD despite no products being licensed for this purpose. The practice was regarded as acceptable on the cascade, however, more recent scrutiny of this practice has determined this use would rarely, if ever, have satisfied cascade rules. The use of antibiotic footbaths has also been identified as a significant contributor to antibiotic use on farms, making their use irresponsible (Hyde et al, 2017a, b), especially since there is little evidence to support their efficacy. Overall, the veterinary profession was unable to support continued use of antibiotic treatment baths, instead advocating a move towards individual treatment (Bell et al, 2017). As for all causes of lameness, prompt individual treatment of BDD lesions (within 48 hours) is important for reducing lameness prevalence on farms (Barker et al, 2010). It can also prevent transition to the M4 stage, which is responsible for most transmission and perpetuating this endemic disease (Biemans et al, 2018).
All lesions should be cleaned, dried, and debrided (for example by wiping hard with dry cotton wool) to stimulate an inflammatory response to create a healthy granulation tissue bed, before application of an antibacterial product (Bell and Vanhoudt, 2020). There is little evidence that systemic use of antibiotics is superior to topical applications, and therefore topical antibiotic treatments are recommended to avoid increased medicine costs and withdrawal periods (Laven and Logue, 2006a). Licensed topical antibiotic treatments in the UK are oxytetracycline and thiamphenicol sprays. It is possible that thiamphenicol is slightly more effective in terms of cure rates 28 days post treatment (Holzhauer et al, 2017). Unlicensed treatments should be avoided as they often use larger doses of antibiotics which result in the presence of antibiotic residues in milk. Care must be taken not to contaminate the udder/teats during treatment, as it is possible for this to cause contamination of milk and necessitate application of a withdrawal period (Cramer et al, 2019).
There are also a variety of topical pastes and non-antibiotic treatments available, often with no published evidence to support their use. There is one product containing chelated copper and zinc (Intra Hoof-fit Gel, Intracare, Veghel, Netherlands) that is licensed for use in the UK (Bell and Vanhoudt, 2020). This product has been found to have comparable or superior efficacy for treatment of M2 lesions compared with chlortetracycline spray (Holzhauer et al, 2011; Klawitter et al, 2019). Regardless of the treatment selected, lesions should be checked, and treatments repeated (as detailed in the summary of product characteristics (SPC)) daily until a scab has formed.
Bandaging lesions has been shown to improve the probability of cure of M2 lesions (Toholj et al, 2012; Klawitter et al, 2019) and prevent M4 lesions from developing (Klawitter et al, 2019), however the latter study employed weekly bandaging using a four-layer waterproofed bandage for up to 4 weeks, which is unlikely to be practical for widespread adoption. Instead, a single bandage applied for 12 hours (or until the next milking) is suggested as a compromise to improve contact between topical treatment and lesion without risking injuries from prolonged bandage use (Bell and Vanhoudt, 2020). However, the evidence for bandage use remains weak and cure rates after single application of oxytetracycline with a simple bandage used were low when trialled (13.8% for primiparous and 38.7% for multiparous cows) (Nishikawa and Taguchi, 2008). Repeat treatments of licensed products administered according to their SPCs should be prioritised.
Foot disinfection
Foot disinfection is achieved using footbathing, which is aimed at preventing M4 lesions from becoming M4.1 lesions (Döpfer et al, 2012). M2 lesions are best treated individually, as discussed above, as footbath disinfectants risk drying out wound edges and delaying healing (Holzhauer and van Egmond, 2021). (However, given the difficulties in diagnosing individual lesions outlined in this article, it is likely that many active lesions will be ‘treated’ only through footbathing of the herd).
Footbath design
Studies have reported wide variation in footbath dimensions; however, it has been recommended that the optimum length for ensuring at least two immersions of each rear foot is 3.0 m, while a 3.7 m length significantly increases the number of feet with three or four immersions (Cook et al, 2012). Footbath volume (which contributes significantly to the volume of liquid waste entering slurry management systems) can be minimised by reducing width to 0.6 m, which has been shown to be well-tolerated by cows (Cook, 2017). Step-in height is also important for increasing the number of foot immersions and reducing losses from the footbath and therefore the cost of maintaining it: 0.28 m is recommended (Cook, 2017; Ariza et al, 2019). The depth of the footbath should be sufficient to immerse the whole foot including the skin-horn junction on the dorsal aspect. A 12 cm solution depth is recommended, however, in the author's experience solution depth as low as 8 cm may be sufficient, but this can only be gauged by observing cows walking through the footbath (Agricultural and Horticultural Development Board (AHDB), 2019).
There is some debate regarding the use of prewash footbaths. Received wisdom indicates that this would enhance foot cleanliness, reduce contamination of the subsequent treatment bath, increase contact between treatment bath disinfectant and foot skin, and thereby improve prevention and treatment of BDD lesions. Information on the effect of prewash footbaths on BDD prevalence is lacking, however they do reduce organic matter concentration in treatment baths (Manning et al, 2017), most likely as a result of fewer defecations in the treatment bath (Ariza et al, 2019).
Footbath frequency and footbath renewal
A recent study observed a wide variety in frequency of footbathing from once a month to once daily, with a median of three times weekly (Cook et al, 2012), however footbathing as often as every day is practiced on some farms (Blowey, 2005). There are no clear industry guidelines on frequency of use, however 3–4 times weekly appears to be optimum in terms of balancing disease control with the cost of footbathing, and can be adjusted every 6–8 weeks for individual farms depending on results.
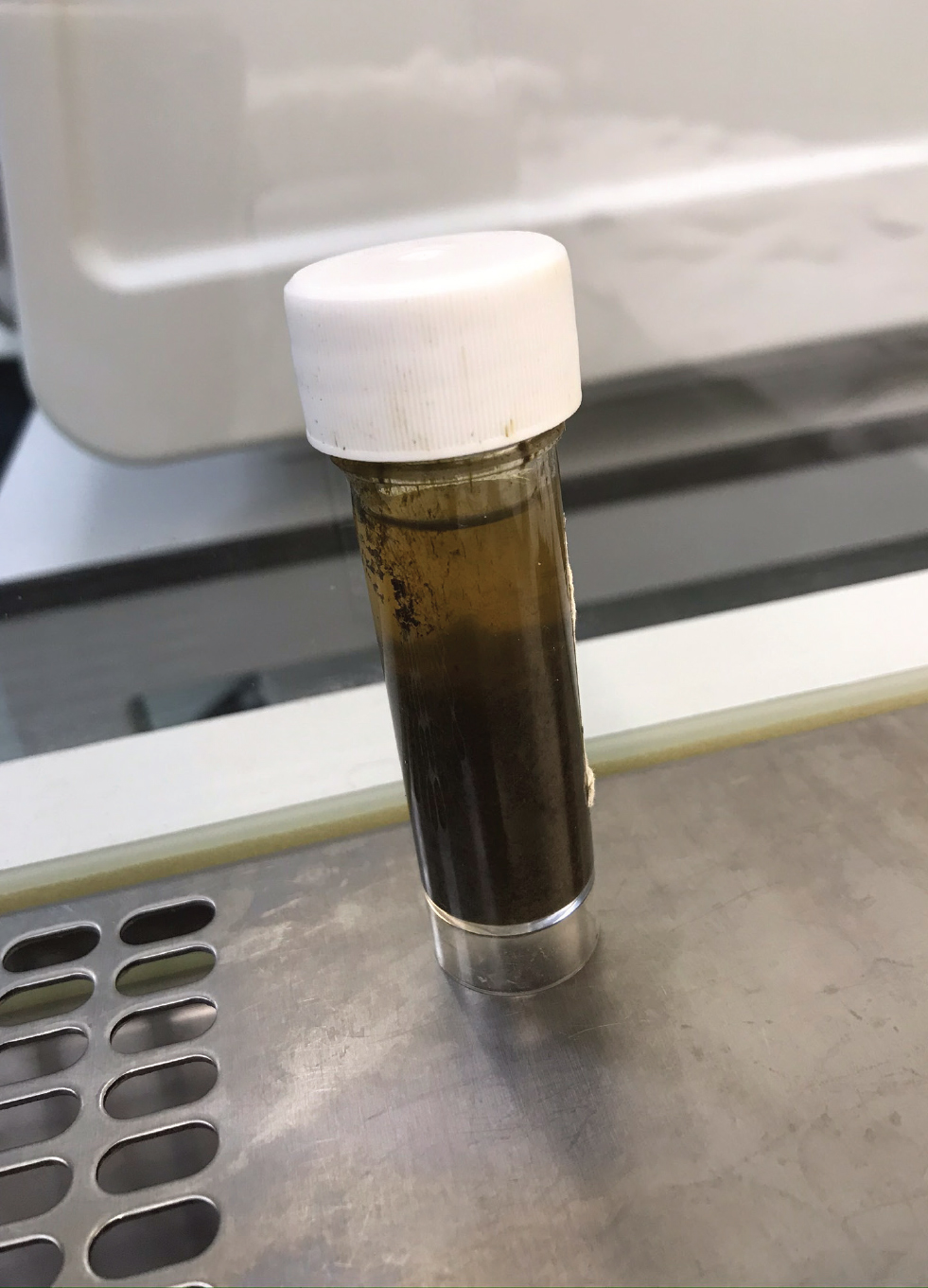
Empirical advice on the frequency of footbath replenishment usually recommends changing the solution every 100–300 cows depending on footbath size, which roughly equates to 1 litre of solution per cow passage (Cook et al, 2012). Biocides approved for veterinary usage are required under EU Legislation (Regulation EU No 528/2012) to show efficacy against Enterococcus hirae, Proteus vulgaris, Pseudomonas aeruginosa and Staphylococcus aureus after exposure to up to 20 g/litre of organic matter. Although this testing does not include the Treponemes that are important in development of BDD, it has been shown in vitro that these are susceptible to a range of common biocides in the presence of 20% manure contamination (Hartshorn et al, 2013). It is assumed that the level of contamination would not normally exceed this threshold if solutions were changed at the rate of 1 litre per cow passage. This may not be adequate on every farm since the main influence on footbath cleanliness seems to be defecation in the footbath, which differs between farms (Ariza et al, 2019). Figure 1 shows a sample taken in a scenario where footbath volume exceeded 1 litre/cow, but contamination was heavy nevertheless. Although the 20 g/litre threshold was rarely exceeded in published studies, the depth of the footbath becomes significantly reduced and therefore this may become the main motivator for timing of renewal instead (Manning et al, 2017; Ariza et al, 2019).
Footbathing disinfectants
Previous surveys have shown copper sulphate and formaldehyde to be the most used antibacterial agents, and often farms will use both (Cook et al, 2012; Solano et al, 2015). There are many limitations to the available evidence regarding chemical efficacy, however there is a consensus that 4–5% copper sulphate is effective for reducing prevalence of BDD lesions. This paucity of scientific evidence for efficacy was highlighted in a recent meta-analysis of footbath protocol trials which concluded that only 5% copper sulphate used at least four times weekly was superior to no footbath or water only for treatment of BDD. Furthermore, there was no published evidence that any agent/regimen was superior to water or nothing for prevention of BDD (Jacobs et al, 2019).
Both copper sulphate and formalin use have significant drawbacks. The former may accumulate in the soil and have long-term toxic effects in the environment, while the latter is a known carcinogen with defined occupational exposure limits (0.3 parts per million (ppm) long-term exposure value in the European Union) (Laven and Logue, 2006b; Speijers et al, 2010). Certainly 0.3 ppm is frequently exceeded in the vicinity of the footbath, especially during filling and emptying, and formaldehyde concentrations in the air increase on warmer days and if ventilation is not adequate (Doane and Sarenbo, 2014). Although the Red Tractor Assurance scheme bans the use of hoof care products containing quarternary ammonium compounds (Red Tractor, 2021), to the author's knowledge there is currently no governance on formalin or copper sulphate use from milk buyers or farm assurance schemes. The author would argue that there are few cost-effective alternatives therefore copper sulphate or formalin use is currently essential to maintaining good animal welfare. Acidified copper sulphate (which results in a lower copper content of 2%, compared with the 4–5% usually recommended) appears to be at least equivalent to formalin for prevention and treatment of lesions (Holzhauer et al, 2012a), however it should be ensured that the pH of the footbath remains above three or there is a risk of causing further proliferative lesions (Cook, 2017).
It cannot be assumed that the intended chemical concentration of a footbath and the actual concentration are the same. One study found that formalin concentrations in footbaths that were meant to be 4% concentration varied from 1.2–6.9% after one passage of the herd (Holzhauer et al, 2004). Another found 3% formalin where the producer believed the footbaths were 5% formalin solution (Doane and Sarenbo, 2014). Errors occur as a result of inaccurate measuring of the footbath or variation in filling depth, and these should be reviewed regularly. AHDB has published a footbath capacity guide which provides a quick reference tool for ensuring footbathing biocides are diluted correctly (AHDB, 2020).
Footbathing non-milkers
BDD is not a disease restricted to milking cows. A Canadian study identified BDD in youngstock on 11 of 28 farms and recorded 11% prevalence in heifers over 12 months old (Jacobs et al, 2017). A Dutch study showed the prevalence in heifers less than 1 year old was just 0.4% but increased to 12.9% between 1 year old and first calving. Presence of BDD in youngstock is associated with increased risk of BDD after calving (OR 5.97, 95% CI 3.01–11.81) (Laven and Logue, 2007; Holzhauer et al, 2012b). Furthermore, developing BDD during the rearing period has detrimental effects on milk production (up to 335 kg) and days open (mean increase in of 24 days) (Gomez et al, 2015). This area of BDD control is often neglected as footbathing heifers is usually inconvenient; many farms would benefit from investing in footbathing facilities for heifers. Concrete footbaths can be added to housing externally. As in the example in Figure 2, this might not afford an opportunity for optimum design, but is still likely to improve foot hygiene and reduces BDD cases. There is little data about BDD in dry cows, however one study found that 30% of dry cows have BDD lesions and therefore should also be footbathed (Bay et al, 2021).

Approach to reviewing bovine digital dermatitis management with clients
It has been shown that a thorough risk assessment about BDD and provision of high-quality advice is insufficient to provoke action (Vanhoudt et al, 2021). It is recognised that using a motivational interviewing style to identify a farmer's motivations and communicating advice in a client-oriented manner improves outcomes. Regular follow-ups at pre-agreed intervals are also useful (Holzhauer and van Egmond, 2021). Given the challenges outlined in this article, the author proposes the approach outlined in Box 1 for improving BDD management on farms.
Box 1.Approach to improving bovine digital dermatitis managementHow is bovine digital dermatitis (BDD) diagnosed on this farm, and could this be improved?
- Accepting that it is impractical for a farmer to check all feet in the foot-trimming crush regularly, could they be persuaded to check for lesions in the parlour weekly? If this cannot be accommodated during milking because of the extra time or member of staff needed, scoring cows in headlocks, or even freely moving in housing may still be better than no active process for diagnosis at all.
What treatment protocols are in place for individual lesions?
- Are repeat treatments being administered, and is it possible to safely incorporate bandaging into the protocol?
Footbathing — audit the following:
- Dimensions of the footbath
- Frequency of use
- Frequency of renewal — take a sample to look at organic matter content and observe depth of footbath solution at the end of use
- Biocide concentration — observe filling of the footbath and use the dimensions to check the biocide concentration and pH if equipment is available
- Footbathing of heifers and dry cows
Reviewing BDD prevalence and adjusting protocols
- Review BDD prevalence within 6–8 weeks to assess the efficacy of any changes made so that protocols can evolve depending on response
Conclusions
BDD is endemic and highly prevalent in many UK dairy herds. Encouraging protocols for active diagnosis, implementing best practice for individual treatment of acute lesions, and auditing footbathing regimens will reduce the numbers of cows affected. This is important both from an economic and a welfare perspective.
KEY POINTS
- Bovine digital dermatitis (BDD) is an area where there is opportunity for veterinary surgeons to have positive impact.
- Active diagnosis of BDD is needed to identify acute lesions for treatment, thereby reducing prevalence.
- Implementing an individual treatment protocol for acute lesions improves cure rate and reduces the number of cases which become chronic.
- Improvements to footbathing regimens can often be made by reviewing chemical concentration and timing of footbath renewal.
- Regular follow-up is key to assessing the impact of changes made and for engaging clients in the disease control process.


