Sheep scab, a highly contagious skin disease caused by infestation with the ectoparasitic mite Psoroptes ovis, continues to pose a serious threat to the welfare and productivity of the UK sheep industry (Figure 1). Characterised by severe itching, wool loss, and open wounds resulting from self-excoriation, the disease inflicts significant distress on affected animals, leading to substantial economic losses estimated at £80–200 million annually (Nixon et al, 2020). An infestation can be started through the transfer of a single fertilised female mite and once on the animal, the mites located on the skin surface, where they abrade the skin surface with their mouthparts, depositing faecal pellets, which contain several allergens, i.e., Pso o 1, Pso o 2 homologous to house dust mite allergens (van den Broek and Huntley, 2003). This combination of skin abrasion and deposition of pro-inflammatory allergens results in cutaneous inflammation and production of a serous exudate, which the mite uses food source. The life cycle of P. ovis progresses from egg> larvae> protonymph> tritonymph> adult (male and female) with all stages being completed on the host, and full progression taking between 11–19 days. Adult females can live for up to 42 days, each laying 15–30 eggs. Once infested, there is a lag phase, typically lasting ~10 days, during which time early lesions begin to develop, and the mite population increases in number(van den Broek and Huntley, 2003). This progresses into an exponential growth phase, characterised by rapid lesion expansion, with the mite population also increasing rapidly, doubling every ~6 days. Lesions are characterised by yellowish scabs, formed as the serous exudate dries, resulting in the staining of the base of the fleece. A moist outer ring surrounds the lesions, and this area contains most of the actively feeding mites, which radiates outwards in a centrifugal fashion, triggering an inflammatory response on naïve skin at the leading edge of the lesion. As lesions continue to expand, they cause intense pruritus, with the host responding by nibbling and scratching at their fleece, resulting in wool loss, reduced weight gain, and low birth weights in lambs (Figure 2). In severe cases, loss of condition can be more extreme, resulting in depression, emaciation and even death. As an obligate parasite, P. ovis relies on the interaction with the host to progress through their life cycle. However, they can survive off the host for up to 17 days, where they can be picked up by a new host on fleece tags left on fences or handling equipment, infested clothing items, shearing combs etc.


Although cases of sheep scab can be seen throughout the year, it is predominantly a disease of the autumn and winter, with the majority of cases occurring between November and March. This is partly due to the thicker fleeces present at this time of year, which provide a more suitable environment for mite survival (i.e., low UV light levels and high humidity). However, increased animal movements (i.e., ram sales) and higher stocking densities, placing animals in closer proximity also contribute to the increased incidence at this time of year. In most cases, given time, infested animals will recover as they develop a natural immunity to the infestation. However, this immunity is not sterile, meaning they can remain infested but not exhibit clinical signs whilst still being a risk to other animals. In these cases, the mites can persist in the cryptic sites, i.e., inguinal and infraorbital fossae and the external auditory canal. All breeds of sheep can be infested with scab, but some breeds appear more susceptible to infestation, with lowland breeds considered more susceptible than upland breeds. However, the greatest variation in response to infestation is still at the individual level, with some sheep responding more severely to infestation than others.
In most cases, given time, the infested animals will recover as they develop a natural immunity to the infestation. However, this immunity is not sterile, meaning they can remain infested, but not exhibit clinical signs, whilst still being a risk to other animals. In these cases, the mites can persist in the cryptic sites, i.e., inguinal and infraorbital fossae and the external auditory canal. All breeds of sheep can be infested with scab, but some breeds appear more susceptible to infestation, with lowland breeds considered more susceptible than upland breeds. However, the greatest variation in response to infestation is still at the individual level, with some sheep responding more severely to infestation than others..
Despite extensive eradication efforts in the mid-20th century, sheep scab re-emerged in the UK following its reintroduction in 1973 via imported sheep from Ireland. The initial eradication campaigns, which relied on compulsory dipping, successfully reduced scab incidence to negligible levels. However, deregulation in the 1990s, coupled with inconsistent treatment practices, allowed the disease to become endemic once again, being particularly prevalent in hill and upland farms where there are areas of common grazing. Some commentators have noted that this may have been exacerbated by the introduction of the first endectocide (ivermectin) as the product requires two injections 7 days apart to be fully effective. The practicality and cost involved meant that many flocks received only the first dose, which suppressed clinical signs but failed to eliminate the infestation, allowing sub-clinically infected sheep to be moved around the country. Clinical disease is currently reportable (gov.uk, 1997) in England and Wales, while in Scotland and Northern Ireland, where animal health is devolved, sheep scab is notifiable under the Sheep Scab Order (Scotland) 2010 (gov.uk, 2010) and the Sheep Scab Order (gov.uk, 1970), respectively.
Various factors have contributed to the persistence of sheep scab. One significant challenge has been the recent development of resistance to the macrocyclic lactone (ML) injectables, a common treatment method for sheep scab that is also heavily relied upon for the control of gastrointestinal nematode (GIN) infections in sheep. In 2017, the first ML-resistant strains of P. ovis were confirmed in the UK (Doherty et al, 2018; Sturgess-Osborne et al, 2019), necessitating a renewed focus on alternative treatment strategies, particularly the increased use of organophosphate (OP) plunge dipping. The effectiveness of OP dipping, combined with advancements in diagnostic methods, provides new opportunities for managing and controlling the disease more effectively. However, the use of jetters and showers for scab treatment may also further the development of OP resistance.
Traditional diagnostic methods, such as skin scrapes examined under a microscope, often fail to detect infestations until they are well-established, delaying effective treatment and allowing the mites to spread between animals and flocks (Ochs et al, 2001). Recent innovations, such as the development of an enzyme-linked immunosorbent assay (ELISA) blood test for the detection of sheep scab (Nunn et al, 2011; Burgess et al, 2012), significantly improve the early detection of sheep scab, with a test sensitivity of 98.5% and specificity of 97%. The ELISA test, developed by the Moredun Research Institute, detects antibodies to P. ovis as early as two weeks post-infestation, enabling timely and targeted interventions (Hamer et al, 2019).
Addressing sheep scab requires a multifaceted approach that includes stringent biosecurity measures, accurate diagnosis, appropriate treatment, and coordinated control efforts among farmers. Biosecurity practices, such as quarantining new arrivals and ensuring the cleanliness of transport and handling equipment, are critical to preventing the introduction and spread of scab within flocks.
Recent projects across the UK have demonstrated the effectiveness of coordinated control strategies in reducing the incidence of sheep scab. These initiatives, supported by various funding bodies and involving collaboration between farmers, veterinarians, and researchers, highlight the potential for collective action in managing this persistent disease. For instance, in England, the RDPEfunded ‘For Flock's Sake’ project successfully identified scab hotspots and implemented coordinated treatments using blood testing. Similar efforts in Scotland, Northern Ireland and Wales have shown promising results in controlling scab through regional cooperation and strategic interventions.
The future of sheep scab control lies in continued innovation and collaboration. Ongoing research into the development of a pen-side blood test and a future sheep scab vaccine offers hope for more efficient and effective management tools. In particular, a commercially available vaccine has the potential to revolutionise the control of sheep scab by providing long-term immunity and reducing the current reliance on chemical treatments.
The long-term control of sheep scab in the UK depends on a comprehensive approach that combines biosecurity, early diagnosis, appropriate treatment and collective action. Advances in diagnostic methods and the potential for future vaccines represent significant steps forward in managing sheep scab. Continued support for testing and coordination at regional and national levels will be crucial to achieving sustainable control of sheep scab, safeguarding the health and productivity of the UK sheep industry.
Key sheep scab information Pathogen
Sheep scab, or psoroptic mange, is caused by infestation of the skin surface with the scab mite, Psoroptes ovis. The mite can survive off-host for 16–19 days, and sources of infestation include anything the infested sheep has contacted, such as, fence posts, trees, equipment, trailers and anyone handling the sheep
The disease
Sheep scab It is one of the most contagious endemic parasite diseases affecting sheep, scab is present throughout the year, but the majority of outbreaks occur between September and March
Symptoms
The disease is characterised by crusty yellow scabs on the skin surface and is accompanied by restlessness, scratching, loss of wool, bleeding wounds and loss of condition
Impacts
Reduced animal performance (loss of ewe condition, poor lamb growth rate, reduced quality skins and wool damage) and significant welfare problems. Financial cost estimated at £80–200 million annually for the UK sheep industry
Treatments
Limited to macrocyclic lactone (ML) injectables and organophosphate (OP) plunge dipping. The presence of mites resistant to the ML injectables was confirmed in 2017 with further spread across the UK.
Diagnosis
Accurate diagnosis is crucial to ensure that the correct treatment is given at the right time. For example, other skin infections or infestation by multiple ectoparasites can affect treatment selection. Diagnosis is classically performed by a skin scrape, but sensitivity can be low and often fails to detect sub-clinical disease. A diagnostic blood test (ELISA) for sheep scab, can diagnose the disease before clinical signs appear
Traditionally relied on skin scrapes, now improved with the availability of a blood test for early detection. Sheep can appear clinically normal when first infested, making early detection difficult, with the sub-clinical spread of scab being a significant problem
Control
Scab is difficult to control due to its rapid spread through direct contact and the easy transfer of mites. The effective use of the remaining chemotherapeutics, particularly the OPs, for scab control and coordinated control efforts are crucial to ensure that we maintain their efficacy
Keeping scab out
Good biosecurity, such as well-maintained double fencing, can prevent the introduction of sheep scab into a flock by preventing direct contact with neighbouring flocks. Test all incoming stock to see if treatment is required, quarantine for at least two weeks and observe for signs of infestation
Legislation
Sheep scab is notifiable in Scotland and Northern Ireland under The Sheep Scab (Scotland) Order 2010 and The Sheep Scab Order (NI) 1970, respectively. In England and Wales, the Sheep Scab Order 1997 addresses the movement and treatment of sheep affected by sheep scab.
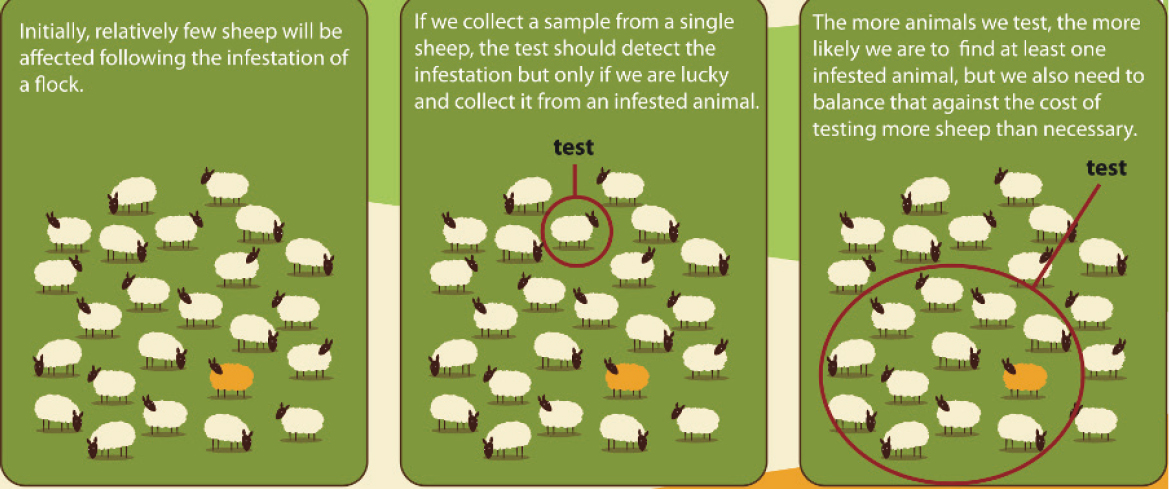
Keeping sheep scab out: effective biosecurity
In addition to the high risks of sheep scab associated with the use of common grazing (Rose et al, 2009; Rose and Wall 2012; Chivers et al, 2018), movements of sheep from farm to farm or through markets are significant factors in the spread of sheep scab. Therefore, biosecurity should always be the first line of defence against scab (Moredun, 2016). Previously, farmers were advised to assume that all purchased or returning sheep were potentially infested with sheep scab and should, therefore, be treated. However, following the introduction of a sheep scab blood test to the tools available and the emergence of mites resistant to the ML treatments, we should now aim to test sheep while they are in isolation and then only treat if required. This fits with general advice to quarantine animals for at least 3–4 weeks, allowing 2 weeks to elapse before blood samples are taken providing sufficient opportunity for infested animals to seroconvert and generate anti-P. ovis antibodies The sheep scab blood test (ELISA) is designed as a flock-level test, and it is recommended that a minimum of 12 animals be tested from each flock or management group.
Additional biosecurity measures include ensuring that any contractor's equipment, including clothing, coming onto the farm is clean and sufficiently disinfected; transport is thoroughly washed out, and where possible, sheep are prevented from contact with neighbouring flocks using double fencing. Adequate fencing is an effective means of keeping sheep scab out of a flock. Ideally, using double fencing where practical (at least 1 metre apart) and especially at high-risk boundaries, where the farm borders with other farms, common grazing or forestry.
Diagnosis of sheep scab
Effective diagnosis of sheep scab involves a combination of clinical examination and blood testing. Given the complexity of diagnosing sheep scab, the early involvement of the vet is highly recommended, as they provide expertise in distinguishing scab from other diseases and can recommend appropriate diagnostic and treatment options. Timely diagnosis is crucial to facilitate rapid and appropriate treatment, preventing the spread of the disease both within and between flocks. Suspicion of a sheep scab infestation is often triggered through the presence of clinical signs, with sheep demonstrating intense itching, wool loss and the presence of scabs and lesions on the skin. Itching can become severe and increasingly persistent, leading to significant distress in affected sheep. Infested sheep often exhibit behaviours such as rubbing against objects (fence posts, trees, hedges, etc), biting at their flanks, scratching with their hind legs or neck arching. Animals can also exhibit a nibble (hypersensitivity) response during examination, which can be very characteristic of sheep scab. These behaviours are a response to the severe irritation caused by the mites and often worsen with time.
Clinical examination
Sheep scab is classically diagnosed by taking skin scrape samples from suspected lesions, followed by microscopy to confirm the presence of P. ovis mites (Figure 3). While this method of diagnosis is particular for sheep scab, the sensitivity can vary (as low as 18%) due to difficulties in identifying early lesions and operator variability in the skills required to obtain satisfactory samples and identify the mites (Ochs et al, 2001). This results in many cases of scab not being detected until there is a very high level of clinical disease with the associated production losses and the risk that the disease has already spread to neighbouring flocks. In this case, the presence of mites in skin scraping samples examined via microscopy should be considered a positive result for sheep scab. However, due to the low sensitivity of this method, an absence of mites on a skin scrape does not necessarily rule out a scab infestation, and a blood test should be considered in the presence of clinical signs, behavioural changes or suspicion of infestation. Sheep scab can be confused with a lice infestation, resulting in intense pruritus, scratching and wool loss. However, animals in good condition often keep lice in check, with severe lice infestations often observed in poorly conditioned animals. The two diseases can be differentiated through skin scraping, with the presence of lice or mites confirmed through microscopy. It is also possible for an animal to be infested with lice and sheep scab simultaneously.

Collection of mites via skin scraping is a skilled technique and should be carried out to maximise the possibility of identifying mites. Begin with a thorough clinical examination, checking for wool loss or areas of discomfort, particularly where the fleece has become discoloured, feels damp to the touch or dirtied through scratching with a hind leg. In these areas, a more thorough examination of the skin surface by palpation should be conducted to locate lesions (scabs/crusts). Some animals will respond with a nibble reflex (hypersensitivity response), a good indicator of infestation. Mites are more likely to be found around the moist leading edge of the lesion where they meet naïve skin. If no lesions can be found, the cryptic sites, such as the infra-orbital fossae, pinnae of the ear, crutch/perineum and inguinal fossae (van den Broek and Huntley, 2003)should also be examined. Before taking a skin scrape, remove excess fleece down to the skin level using curved surgical scissors; this can be placed in a ziplock bag or universal container for submission alongside the skin scrape. Using a fresh disposable scalpel blade held at ~90 degrees to the skin, take a scraping from the leading edge of the lesion, shaving rather than scraping the skin; blood should not be drawn using this technique. If required, take multiple samples from each animal and pool these for submission. To prepare the skin scrape sample for submission, carefully scrape the scalpel blade across the inside of a plastic universal container to remove the lesion material and then safely dispose of the scalpel blade.
Sheep scab blood testing (ELISA)
Scientists at the Moredun Research Institute, Edinburgh, have developed a commercially available blood test (ELISA) for sheep scab that allows for early detection before clinical signs are apparent (Figure 3) (Nunn et al, 2011; Burgess et al, 2012). This means that scab can now be identified before it has spread, facilitating targeted, coordinated treatments to achieve long-lasting scab control. The blood test detects antibodies (IgG) in sheep blood specific for a unique P. ovis mite allergen (Pso o 2), meaning that the test can accurately determine if an infestation is due to the scab mite or another ectoparasite, i.e., lice, which does not cross-react with the test (Figure 4). This is crucial as the treatments for different ectoparasites can vary, with MLs not being effective against lice and pour-ons used to control lice not being effective against sheep scab.
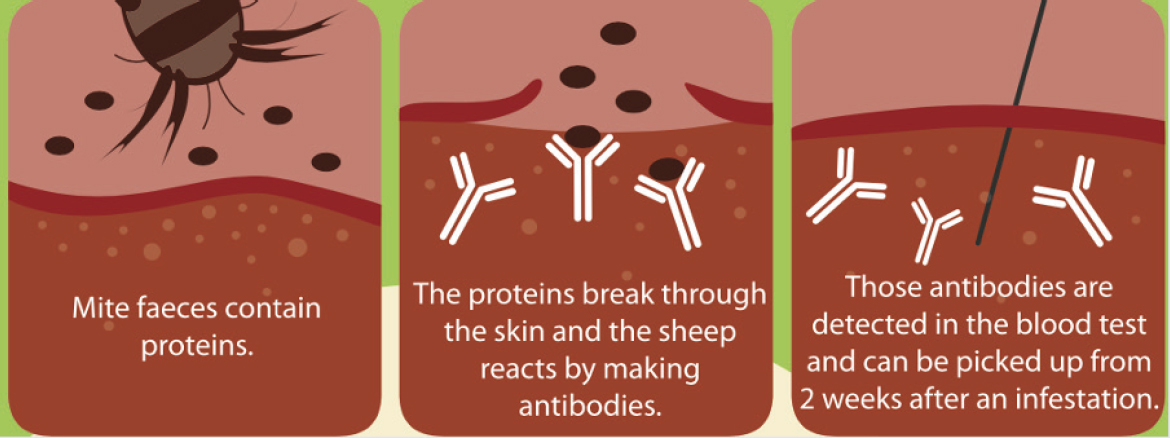
The test detects scab within 2 weeks of an infestation and before the onset of clinical signs. This is important in subclinical disease, which represents a significant problem in the control and spread of sheep scab (Hamer et al, 2019). Once an animal has become infested, it can take weeks or months before they exhibit clinical signs, and this is due to a significant lag period (van den Broek and Huntley, 2003) in the development of the lesion, which occurs due to the small number of mites involved in seeding the initial infestation. Following exposure to the host, mites locate themselves on the skin surface, releasing pro-inflammatory factors, some of which are allergens. This triggers an inflammatory response, accompanied by the production of a serous exudate, that the mites use as a food source. As this exudate dries, it forms the scabs by which the disease is known. The mite population and lesion development slowly increase. Still, depending on several variables, i.e., location of the initial infestation, fleece density and depth, climatic conditions and the degree of self-grooming undertaken by the host, lesion expansion may take weeks or months, thus delaying the advent of clinical signs.
In contrast, the blood test can detect disease within 2 weeks of infestation, once the animal has seroconverted. The test is designed to be used at the flock or management group level, with a minimum of 12 animals sampled from each group. The test has a sensitivity of 98% and specificity of 97.5%, providing a 95% accuracy of detecting sheep scab should the flock be infested based on an assumed prevalence of 20% (Figure 5).
Treatment of sheep scab
Following a sheep scab diagnosis, under UK sheep scab legislation, the owner/keeper must treat with an approved product or move animals to slaughter, adhering to the strict movement restrictions enforced where scab is confirmed (see Table 1). The owner/keeper must also warn neighbouring farms and let them know when treatment will begin. This allows cooperation and coordination of treatments to ensure that all adjacent flocks are treated within a 2–3-week period, making the most of residual protection provided by the treatment. All animals must be treated, including both affected animals and all other animals that may have been in contact. If shared or common grazing is used, then all sheep belonging to all owners must be treated. If feral sheep are present, then they must be gathered and treated or culled. In addition, the suspected source of the infestation should also be alerted so that treatment can be administered.
| Active | Product name(s) | Application method | Protection period for sheep scab | Withdrawal period (days) | Other ectoparasites treated |
|---|---|---|---|---|---|
| OP - Diazinon | Gold fleece | Plunge dip | At least 8 weeks | 49 | Lice, Keds, Blowfly & Ticks |
| Ivermectin | Ivomec classic |
Subcutaneous Two injections required to treat sheep scab | None, treatment only Clean pasture and segregation from untreated sheep post-treatment required | 37 or 42 Check product | Nasal bots |
| Doramectin | Dectomax | Intramuscular | None, treatment only Clean pasture and segregation from untreated sheep post-treatment required | 70 | Nasal botsx |
| Moxidectin 1% | Cydectin 1% |
Subcutaneous Two injections 10 days apart required to treat sheep scab | 28 days | 70 | Nasal bots |
| Moxidectin 2% | Cydectin 20 mg/ml |
Subcutaneous at base of the ear | 60 days | 104 | Nasal bots |
Before the introduction of the injectable 3-ML (endectocide) products in the mid-1990s, plunge dipping in organophosphate (OP) was the only method available for control of sheep scab. Dips were introduced in the late 19th Century using arsenic and sulphur-based products, followed by organochlorines (OC) after WW2, with the OCs being instrumental in eradicating sheep scab between 1952–72. However, when the scab was re-introduced in 1973, the OP dips were available, joined later by the addition of synthetic pyrethroid (SP) dips. The class and type of ectoparasite treatments used in the UK have changed over the previous 25 years. OP dipping use fell in favour of the MLs from the mid-1990s, along with topical treatments for blowfly and tick control. The SPs were removed from the market amid environmental concerns and mounting cases of resistance in sheep scab mites, and until recently, when the first reports of resistance to the endectocides were reported (Doherty et al, 2018) dipping had become a minority treatment. Following reports of treatment failure using the MLs for scab treatment, populations of P. ovis mites resistant to moxidectin were first identified in the UK in 2017 (Doherty et al, 2018). These were later followed by further cases of ML-resistant mites from Wales and south west England, with resistance being confirmed to all 3-MLs (Sturgess-Osborne et al, 2019). However, it wasn't until cases of resistance in the scab mites were reported that the industry began to realise that a shift back to dipping was required, underlined by confirmation that an OP plunge dip remains completely effective against ML-resistant scab mites (S. Burgess, Personal Communication).
There are now just two options for the treatment and control of sheep scab: plunge dipping in OP or the use of an endectocide (MLs) (Figure 6), and it is unlikely we will see novel treatments in the foreseeable future. The main difference between the scope of these treatments is that OP is active against all ectoparasites affecting sheep; in contrast, the MLs are only effective against sheep scab and nasal bots, meaning that diagnosis is essential prior to endectocide use.

Treatment of sheep scab with MLs:
The MLs offer several advantages over OP plunge dipping, such as increased safety, ease of use, less stress on the animal, reduced need for specialist facilities, and reduced environmental impact. However, these must be weighed against their disadvantages. For example, the narrow anti-ectoparasitic range of efficacy means additional treatments may be required for other co-infecting ectoparasites. Many of the MLs have long meat withdrawal periods, which must also be considered. Following ML treatment, mites are killed in situ, and their faecal allergens and breakdown products may continue to cause irritation and clinical signs for some time. As some MLs do not kill mite eggs or provide lasting protection, they often require multiple doses to kill newly hatching mite larvae. Selecting an injectable ML that provides residual protection long enough to comply with any legislation is important. For example, the Sheep Scab (Scotland) Order 2010 requires that all sheep on the premises be given treatment, providing 16 days of residual protection against re-infestation. If the product used does not provide this, then ensure that treated animals are moved to clean pastures to prevent them from becoming reinfested by mites in the environment. As the MLs are also endectocides, it is important to integrate their use with parasitic nematode control. MLs are broad-spectrum anthelmintics and effective against P. ovis, allowing integrated scab mite control and worming. However, they also provide a means of accelerating selection for anthelmintic resistance in parasitic nematodes if routinely used for scab control. While ML oral drenches are highly effective anthelmintics, they are less than 50% effective against scab when administered by this route and should be avoided.
Guidelines on effectively using endectocides to control sheep scab are available on the Sustainable Control of Parasites in Sheep (SCOPS, no date) website. If using an ML, all sheep in a group/flock must be treated correctly if this treatment is to be effective. Missing one animal or putting them back into an infested area if using a non-persistent treatment (i.e. ivermectin or doramectin) will fail to clear the infestation. In practice, this leads to apparent product failure, which can then be confused with suspected resistance. Guidance on how to deal with these situations is available via SCOPS, including the requirement to report to the VMD under the SARs scheme.
Treating sheep scab via organophosphate plunge dipping
Plunge dipping with an OP remains the most effective method for control of sheep ectoparasites, including sheep scab mites, lice, ticks and keds. To date, there are no reported cases of resistance in scab mites to OP in the UK, but if OP treatments are not applied correctly, then the risk of resistance developing in the future will be increased. Although it can be stressful for livestock, a new breed of mobile contract dippers is becoming increasingly available, which use a caged system to lower animals into the dip carefully. These systems can reduce welfare concerns, and using a contractor can simplify issues around dip purchase and disposal.
Critical elements of effective plunge dipping in OP
The lack of suitable dipping facilities and the costs involved in renewing or repairing dip tanks and maintaining OP disposal licences have led to a significant increase in the use of mobile dipping contractors. To encourage effective dipping, SCOPS has led an industry initiative to develop a Code of Practice for dippers, farmers and prescribers (SCOPUS, 2023).
The need to work together to achieve lasting sheep scab control
In recent years, several Initiatives in the devolved nations of the UK, have demonstrated how collective working can lead to lasting sheep scab control. The first of these was the Rural Development Programme England (RDPE) funded ‘For Flock's Sake’ project, which ran from 2021–23 (Burgess et al, 2024). This project's central ethos was identifying scab hot spots in three areas of England and using the blood test within clusters of farms to identify active sheep scab, followed up with coordinated treatments. The project demonstrated huge enthusiasm and a real willingness to work together from most farmers in the clusters, with >300 farmers participating. Combined with excellent coordinators known to and trusted by the farmers, there was a significant impact on the incidence of sheep scab with year-on-year reductions in flocks testing positive for scab across all three regions. During the first year (2021/2022), 25.6% (±5.5%) of flocks tested positive for sheep scab, while on the second test (2022/2023), just 9% (±3.94%) of tested flocks were positive, showing a highly statistically significant reduction in prevalence overall, but with a strong regional variation (Burgess et al, 2024). Interestingly, issues with persistently infested flocks were identified in the Northern region. Although the blood tests were showing animals were positive for sheep scab, they tended not to show clinical signs of disease at the time of testing. These animals were often managed in areas of common grazing, indicating that in some of these settings, the animals could self-manage the disease, most likely through protective immunity gained from previous infestations. The issue with scab only becomes apparent when animals are moved, or new stock is brought in, with the disease being passed on to these scab-naïve animals. The use of the blood test was key to success as it enabled the identification of infested farms, coordinated timing of treatment and follow-up testing to measure impact. One main output for practitioners will be further developing a risk-based tool to help the interpretation of the flock-level scab ELISA.
In Scotland, a scheme is underway, funded by the Scottish Government, which aims to control sheep scabs on the Western Isles of Lewis & Harris. As part of the project, >100 crofters participated in blood testing during pregnancy scanning in 2023. Testing identified several cases of sheep scab, clustered together in four different areas of Lewis and Harris, and coordinated treatments were then undertaken with MLs just prior to lambing. Flocks across Lewis & Harris then participated in a coordinated OP plunge dipping campaign during the autumn of 2023, using a mobile dipping contractor to coordinate treatments within a short period. In total, ~30k sheep were dipped across ~400 individual crofts/farms, significantly impacting the degree of sheep scab observed during the autumn/winter of 2023/4. Blood testing and treatment were further supported for stock returning to Lewis & Harris in the spring of 2024 following overwintering on the mainland, aiming to limit the risk of the disease returning to the island through infected animals.
In Northern Ireland, a project funded by the Biotechnology and Biological Sciences Research Council (BBSRC) (2022/23) aimed to better understand the extent of the issue with sheep scab, recruiting >100 farmers across Northern Ireland (Adenuga et al, 2024). The project relied on farmers with suspected sheep scab in their flocks, self-reporting to the coordinators. The team then provided free blood testing and treatments, which were coordinated, ensuring contiguous properties were also contacted to limit further disease spread. The project showed that scab is significantly underreported in NI. It also demonstrated that farmers across NI were willing to work with the project team to coordinate efforts to control sheep scab in their flocks. However, additional testing and coordination support was required.
In Wales, the ‘All Wales Sheep Scab Eradication Programme’ started in 2023. It aimed to identify infested farms through self-reporting combined with confirmatory skin scrape analysis. The project covered treatment costs, with technical officers helping to coordinate treatments in ‘index’ farms and surrounding contiguous farms following diagnosis using the sheep scab ELISA (Paton et al, 2022).
Collectively, these schemes have demonstrated that sheep scab is endemic across the UK, with significant levels of underreporting. They have shown that there remains a significant issue with sub-clinical disease, which facilitates the movement of infested animals between flocks. The main positive outcomes from these projects are the ability of the sheep scab blood test to identify infested flocks prior to the appearance of clinical signs and the willingness of farmers to participate, working together with their neighbours to coordinate control efforts. However, for these schemes to have a broader impact on the prevalence of sheep scab across the UK, further support for testing and coordination will be required at both the regional level and across the four nations of the UK.
Future prospects
Pen-side diagnosis
One of the most promising advancements in the fight against sheep scab would be the development of a pen-side blood test. The current ELISA test, while effective, requires laboratory processing, which can delay diagnosis and treatment. The pen-side version, designed for rapid, on-site testing, would use a small blood sample to provide rapid results (less than 20 mins). This innovation will be particularly useful in livestock markets. It will also enable farmers and their vets to make swift and informed decisions about quarantine and treatment, significantly reducing the opportunity for infestations to spread within or between flocks. Rapid diagnosis also supports biosecurity measures by allowing immediate action to be taken when new animals are introduced to a flock, ensuring that infected animals are identified before they have a chance to pass on the disease.
Vaccination
The development of a vaccine for sheep scab represents a significant breakthrough in the long-term, sustainable control of the disease. Moredun has been working towards a sheep scab vaccine and recently tested a prototype in repeated vaccination trials (Burgess et al. 2016). The latest trials have shown that vaccination results in highly significant reductions in lesion size (around 80%) following challenge. This is the greatest reduction in lesion size to date with a sheep scab vaccine, providing encouragement for a sustainable means of sheep scab control in the future. However, to achieve lasting disease control, the vaccine will need to be used alongside existing best practice advice (quarantine and testing) and hand-in-hand with the blood test and existing treatments whilst they remain efficacious.
Conclusions
The future of sheep scab control in the UK is promising, with several innovative strategies on the horizon. The development of a pen-side blood test will revolutionise in-field diagnosis, enabling rapid and informed decision-making. The potential for a sheep scab vaccine offers long-term preventative protection, reducing reliance on chemical treatments and addressing the issue of drug resistance.
Supportive policy and legislation will also be crucial in facilitating these advancements and ensuring their successful implementation. With continued research, innovation, a nd collaboration, the UK sheep industry can look forward to more effective control of sheep scab, safeguarding animal welfare and enhancing productivity for the future.


