Foreword
Effective dry cow management is a crucial part of maximising dairy cow welfare and productivity. It has an impact on calving problems, early lactation metabolic disease, fertility, overall lactation performance and udder health, so getting dry cow management right can set the cow up for a successful lactation It is also one of the areas of farm management where pressure for change is clear. The focus is no longer on the standard 60 day dry period with every cow given dry antibiotics at drying off, instead the focus is on developing a much more flexible system, with shortened dry periods, reduced use of antibiotics and increased use of non-antibiotic teat sealants.
This supplement to Livestock provides a practical guide to some of the key issues associated with developing this flexible system. The first article looks at what the dry period is for with a particular focus on the costs and benefits of shortening the dry period. The next two articles focus on the use of teat sealants and selective dry cow therapy, concentrating not on the science but on the practicalities — how can we increase the use of selective dry cow and internal teat sealants on farm?
Evaluating the effects of shortening, omitting or extending the dry period in dairy cows
The dry period is a critical time at the end of lactation, particularly for cure of intramammary infections. Traditionally it has been set at 60 days but recent literature has experimented with a shorter or absent dry period in order to limit early lactation production, thereby reducing metabolic demand in the post-partum period. One downside is that zero day dry periods are a missed opportunity for cure of intramammary infections and they can result in poorer udder health in the next lactation. This review summarises the evidence on shortening, omitting or extending the dry period, with emphasis on milk production, energy balance and udder health.
The dry period is divided into three phases: involution, steady state and colostrogenesis. Shortening the dry period is most likely to impact on the steady state phase, while omitting the dry period affects all three, as shown in Table 1.
- Involution: this phase involves the cessation of milk production and cure of existing intramammary infections. This is achieved through a combination of cell-mediated and humoral immunity, with or without the addition of intramammary antibiotics. The other key element of involution is the formation of a keratin plug in the teat canal to protect against new infections. The application of teat sealant improves the level of protection.
- Steady state: this is a period of rest for the udder tissue. Infection risk is low due to high concentrations of lactoferrin and immunoglobulins.
- Colostrogenesis: this immediately precedes the next lactation and is characterised by mammary gland development, with associated changes in teat and udder shape. There is systemic production of antibodies which diffuse from the blood into colostrum. ‘Post-parturient immunosuppression’ is driven by hormonal and immune system changes. Towards the end of colostrogenesis there may be some milk leaking which can also increase the risk of new infections.
Table 1. Stages of the dry period and how they might be affected by shortened dry period
| 60 day | 30 day | 0 day | |
|---|---|---|---|
| Involution | 14 days | 14 days | 0 |
| Steady state | 32 days | 2 days | 0 |
| Colostrogenesis | 14 days | 14 days | 2–3 days |
Milk production
Shortening the dry period affects the lactation curve; 30 day dry periods are associated with a delay to peak, and decreased peak yield (Shoshani et al, 2014; van Knegsel et al, 2014). As a result, there is a reduced 305 day milk yield (Church et al, 2008; Watters et al, 2008; Shoshani et al, 2014; Kok et al, 2017), but this has minimal effect on milk constituents (de Vries et al, 2015; de Vries et al, 2016). Although a shorter dry period generally results in a lower volume of colostrum production, the protein content per litre is higher, and there is no effect on passive transfer (Watters et al, 2008; Mayasari et al, 2016; Andrée O'Hara et al, 2019). When cows are exposed to consecutive short dry periods the effect on milk production is less pronounced; one experiment found an average of 40.0 kg/day vs 42.9 kg/day milk production during early lactation (Chen et al, 2016b), although there was no difference in 305 day yield (Chen et al, 2016b).
Omitting the dry period has a bigger impact on milk production, with cows producing significantly less 305 day milk than herd mates with a 30 or 60 day dry period (Annen et al, 2004; van Knegsel et al, 2014; Chen et al, 2016b; Kok et al, 2017). Furthermore, zero day dry periods can result in reduced milk protein percentage, which may affect processing (de Vries et al, 2015). Following a zero day dry period the immunoglobulin levels in milk are increased (Mayasari et al, 2016), but the impact on passive transfer has not been assessed. One study reported that when cows were exposed to consecutive zero day dry periods, 19 out of 39 dried off early (Chen et al, 2016b), which may reflect a physiological importance of a dry period.
It should be noted that the reduction in milk yield is partially compensated by an additional 30–60 days of milk production at the end of the previous lactation, although the overall production over both lactations remains lower (Kok et al, 2017).
Energy balance
There is a large body of research on metabolic health in dairy cattle, and shortening the dry period is just one approach to improving energy balance (Figure 1). Herds should first make sure that nutrition and management are optimised, for further information readers are directed towards a previous article (Cooper, 2017).

The metabolic benefits of a shorter dry period are largely driven by the reduction in milk yield. Several studies have demonstrated improved liver health through hepatic biomarkers and lower serum ketones (Rastani et al, 2005; van Hoeij et al, 2017). The improvement in energy status is also shown by better maintenance of body condition score in early lactation (Gulay et al, 2003; Shoshani et al, 2014; van Knegsel et al, 2014). This benefit of improved energy balance is not seen when cows are exposed to consecutive short dry periods (Chen et al, 2016a).
Omitting the dry period is associated with a greater loss in milk production, and therefore a greater improvement in energy status. Several studies have shown reduced levels of serum ketones and better maintenance of condition relative to 60 or 30 day dry periods (Rastani et al, 2005; Klusmeyer et al, 2009; Mayasari et al, 2017). Similar to the effects on yield, the benefits of omitting the dry period over consecutive years are less pronounced (Chen et al, 2016a).
Udder health
Two of the most important functions of the dry period are cure of existing intramammary infection and prevention against new infections. Involution is a critical phase for both of these functions, and it is largely unaffected by a 30 day dry period. Two UK-based cohort studies concluded that shorter dry periods were not a major risk factor for elevated cell counts or clinical mastitis, and other management factors play a bigger role (Green et al, 2007; Green et al, 2008). Several interventional studies have evaluated udder health after a 30 or 60 day dry period and have found no difference in dry period cure, new infection rate, somatic cell count or clinical mastitis incidence (Church et al, 2008; Watters et al, 2008; van Knegsel et al, 2014; van Hoeij et al, 2016).
While a 30 day dry period has limited impact on udder health, a zero day dry period allows no time for involution, which is a missed opportunity for cure of intramammary infections. One study showed that high cell count cows going directly into the next lactation had a cure rate of 50%, compared with 92% for 30 or 60 day dry periods (van Hoeij et al, 2016). Omitting the dry period has also been shown to increase early lactation somatic cell counts, but not the rate of clinical mastitis (Mayasari et al, 2016; van Hoeij et al, 2016, van Hoeij et al, 2018). At the time of writing, no studies have evaluated the impact of consecutive short or omitted dry periods on udder health.
Extended dry periods
Extended dry periods are commonly used to manage cows with chronic infections or long calving intervals and poor milk production, all of which may be associated with future yield and udder health. These confounding factors mean it is difficult to draw conclusions from retrospective cohort studies. One randomised control trial investigated the effect of a 90 day dry period and found no effect on milk yield but an increase in serum markers of negative energy balance (Weber et al, 2015). To the author's knowledge no studies have assessed udder health following randomly allocated extended dry periods in healthy cows.
Conclusions
Extended dry periods should be reserved only for cows with poor fertility or chronic intramammary infections. Zero day dry periods should be avoided as they are a missed opportunity for cure of existing infections, and are associated with higher cell counts in the next lactation. Furthermore a high proportion of cows will dry off early suggesting that there is a physiological benefit to the dry period. Thirty day dry periods are a better compromise between production and metabolic health, although they should not be used as a cover up for poor nutrition or management. They have been shown to reduce the risk of metabolic disease in the next lactation without negative effects on udder health.
Thirty day dry periods should only be used in herds with good nutrition and transition management. They should be targeted at cows in optimum body condition score (2.75–3.25) and without existing intramammary infection. They should not be used in consecutive years as there are no proven benefits in subsequent lactations. If farmers are using dry cow therapy in combination with a shorter dry period they should consider what product they are using as many have a milk withdrawal beyond 30 days, and detectable levels of antibiotic may persist in milk for longer after calving (Bachmann et al, 2018).
Lastly, farmers and veterinary surgeons should consider routine management that occurs around the dry period for example vaccination, foot trimming, or endoparasite treatment. If shortening the dry period, farmers should carefully plan how these may be affected.
KEY POINTS
- There is no good evidence to support extending the traditional 60 day dry period unless drying off chronically infected or unproductive cows.
- Zero day dry periods should be avoided as they are a missed opportunity for cure of intramammary infections and result in poorer udder health in the next lactation.
- 30 day dry periods are a novel approach to reducing negative energy balance in early lactation, without negative effects on udder health.
- If using 30 day dry periods to manage negative energy balance, they should be targeted at low risk animals in optimum body condition score and without intramammary infection.
References
The use of internal teat sealants as part of selective dry cow therapy — communicating the benefits to farmers
This contribution is aimed to summarise the known benefits of the use of teat sealants, obstacles for their wider use and ways to address farmers' reservations. Internal teat sealants provide protection against the acquisition of new intramammary infections throughout the entire dry period. Their use allows selective dry cow therapy to be effective to reduce antibiotic use yet still prevent new infections. There are significant benefits to their widespread adoption, barriers to their use can frequently be overcome through understanding farmer anxiety and providing education and support.
The change from the lactating to the dry udder and throughout the dry period is a time of increased susceptibility to intramammary infections (IMIs). Traditionally antibiotic dry cow therapy (aDCT) has been used to reduce IMIs during this period, both through the treatment of existing infections and in helping prevent new infections. Internal teat sealants can be used alone to prevent new infections from being acquired during the entire dry period. The use of aDCT is therefore reserved for the treatment of existing IMIs.
The initial process of drying off is followed by a stage of involution. During this stage cows form a keratin plug in the teat canal and the udder produces an iron binding protein (lactoferrin) which deprives bacteria of this essential trace element. This is the time when resistance against acquiring new infections is required and effective elimination of existing infections is possible (Figure 1).
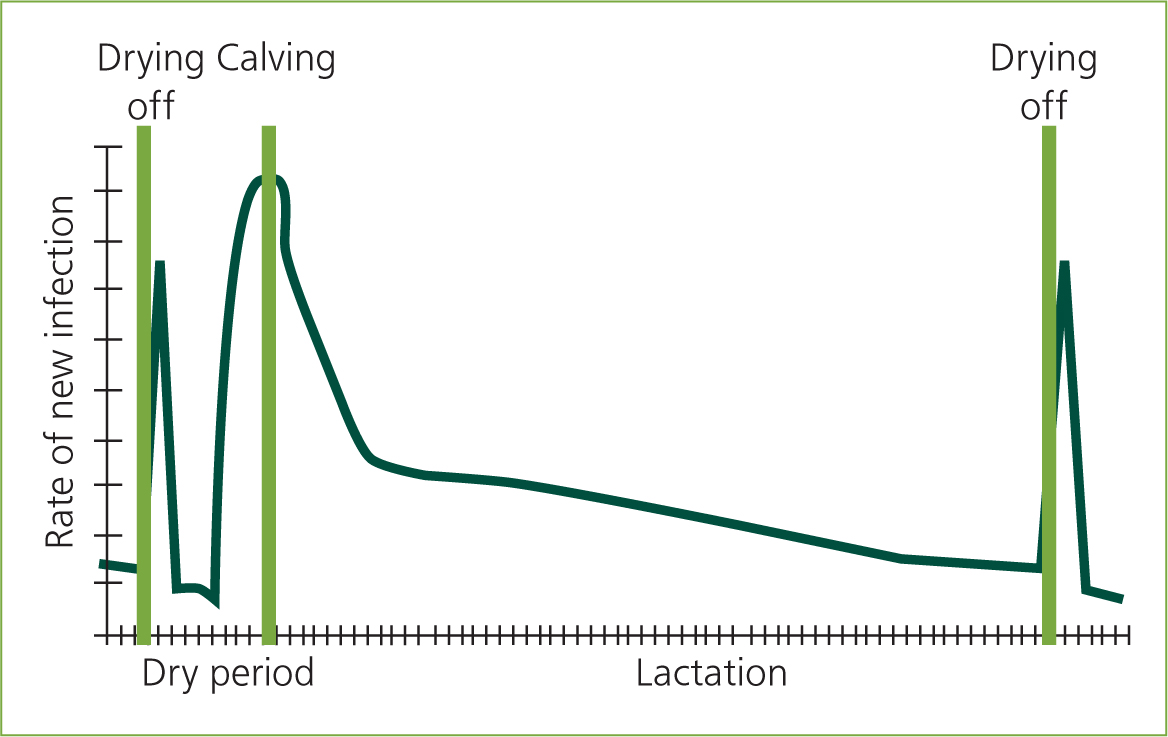
The middle stage of the dry period is a time of steady state when the risk of acquiring a new infection is lower. The keratin plug, if present, is in place and the cell-mediated and humoral immunity is active. Antibiotic given at drying off is starting to decline, ready for the point of calving.
The last stage of the dry period is characterised by colostrogenesis and the change to a lactating udder. This again is a period of high susceptibility, with concentrations of aDCT being too low to prevent new IMIs. This later part of the dry period is therefore the most significant risk period for new IMIs. Internal teat sealants are still present and effective at this stage, preventing the acquisition of new infections throughout the entire dry period.
The importance of the dry period for mastitis parameters in the subsequent lactation has been increasingly recognised in the last 20 years. Green et al (2002) showed that a significant proportion of early lactation clinical mastitis (including those by Gramnegative/coliform organisms) originate from new infections acquired in the dry period. For many farms the dry period is the ‘weakest link’ in mastitis prevention.
What does mastitis cost?
The Agricultural and Horticultural Development Board (AHDB) quotes a figure of £250–300 per individual case of mastitis, this includes milk loss (due to antimicrobial treatment and subsequent lactation loss), costs due to the risk of culling, medicines and time. Milk loss figures, due to the lost yield from the drop in the lactation curve, have been estimated by Wilson et al (2004) for high yielding American Holstein cows as being between about 600 and 1200 kg for the lactation.
These commonly used cost figures do not take into account the effect on other conditions, for example from poor fertility (Hudson et al, 2012). They also do not take into account the cost as a result of transmitting the infection to other cows. Down et al (2013) used computer modelling to predict transmission effect, found to be the most important factor determining the total cost of mastitis, and revised the estimated cost of an average case of mastitis to £430. The total cost, however, is farm specific, and depends on milk price, dominant bacteria, measures to prevent spread, etc; it can vary significantly, but the AHDB figures are increasingly seen as very conservative.
Dry cow therapy
Traditionally blanket aDCT was an essential part of the Five Point Plan, aimed at reducing contagious mastitis. The two main objectives of aDCT were to treat existing intramammary infections and to prevent new ones from being acquired during the dry period.
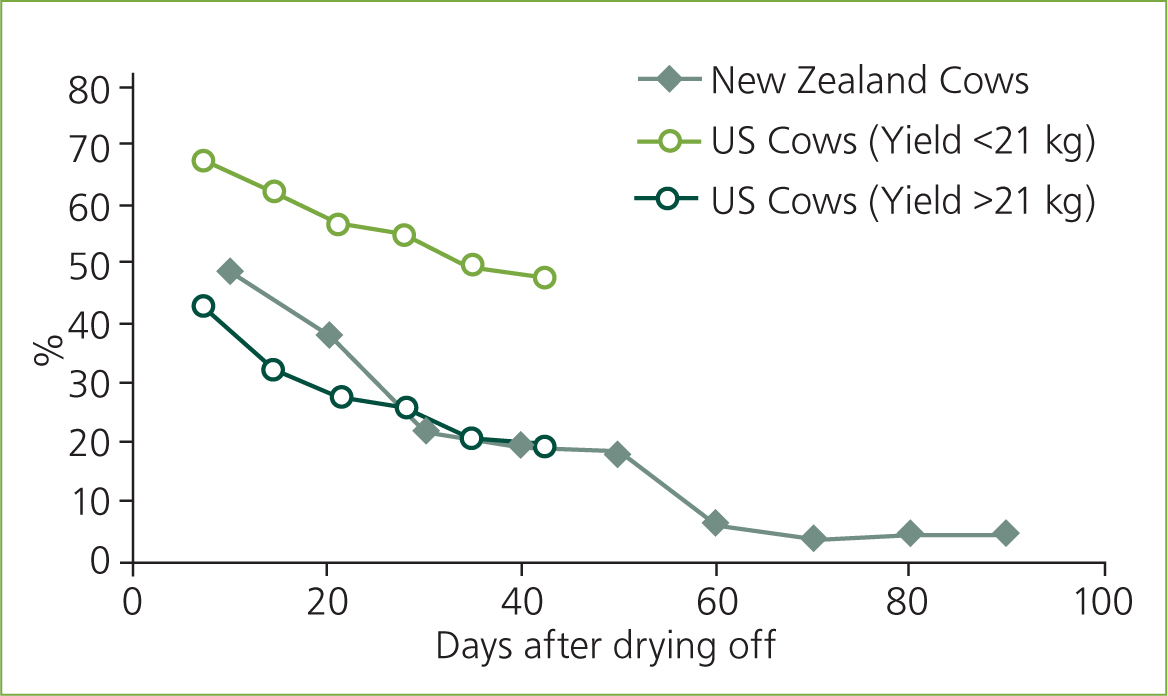
The launch of an internal teat sealant, OrbeSeal® (Zoetis), in the early 2000s changed this ‘dogma’ — internal teat sealants proved to be more effective in preventing new coliform IMIs than aDCT, and as effective for other major pathogens (Huxley et al, 2002). The internal teat sealants work by providing an effective seal of the teat that persists throughout the entire dry period. It has been found that not all cows, particularly those that are high yielding, produce an effective keratin plug (Figure 2). Williamson et al (1995) found that 50% of teats were still open 10 days after drying off and that 97% of clinical dry period IMIs occured in open teats. Similarly Dingwell et al (2004) found 23% of quarters still open 6 weeks into the dry period, again with open teats being a higher risk for IMIs. Milk yields over 21 kg at drying off were a risk factor for open teats, with milk yields still continuing to increase this may become a more common issue.
Is there a disadvantage of using aDCT?
The question as to whether minor pathogens protect against major pathogens is still unanswered (Green et al, 2002; Reyher et al, 2012). There is a lot of recent research into the udder microbiome (e.g. Vasquez et al. 2019), in particular the way commensal bacteria interact and the effect on mastitis. Internal teat sealants, unlike intramammary antibiotics, do not have a direct effect on this microbiome.
Can we just do nothing?
Some organic dairy farmers did not give any intramammary dry cow treatment before the arrival of internal teat sealants. Blanket aDCT is not allowed on organic farms, and prior to the arrival of OrbeSeal there were no other effective preventive measures available. Hovi and Roderick (1998) surveyed organic farms and found that clinical mastitis during the dry period was higher on these farms than on non-organic farms. A high amount (80%) of open teats in the late dry period were found in UK organic dairy herds (Hayton, 2003). The launch of OrbeSeal was therefore particularly beneficial to organic farmers who could not use aDCT for the prevention of new infections.
In summary, internal teat sealants are a non-antibiotic physical barrier providing excellent protection against the acquisition of IMIs throughout the entire dry period. Recent emphasis has been placed on reducing antimicrobial resistance and protecting consumers, which has deservedly gone up the agenda, but more farmers may adopt the use of internal teat sealants and selective dry cow therapy if the direct benefits to the farm are explained in more detail. For example, Scherpenzeel et al (2017) pointed out that blanket aDCT is not the economically optimal approach to management of mastitis during the dry period.
Is there a disadvantage of using an internal teat sealant?
It is known that improper storage or administration of teat sealants can allow the introduction of mastitis causing pathogens into a quarter. This iatrogenic infection in some cases can lead to severe mastitis, and in rare cases to death.
This is a recognised risk, predominantly if no antibiotic is given, and the datasheets of teat sealants put great emphasis on their clean administration and correct storage. The drying off process is a once-a-year event in the cow, and time spent disinfecting the teat to the same standard as in the collection of a milk sample for bacteriology is well paid time (Figure 3). The aim is to prevent IMIs, not to introduce them! A detailed instruction on the drying off routine can be found at AHDB or from the manufaturers of the internal teat sealants. Veterinary surgeons should make themselves familiar with the practical drying off routine and take opportunities to carry out the procedure themselves until confident. This will increase the veterinary surgeon's authority when teaching farmers. It also makes us appreciate how difficult a clean drying off routine can be to achieve in some circumstances, especially with fractious cows, or cows with teat end damage or warts.

A practical drying off training session with farm staff in the parlour can be both enjoyable and educational — for veterinary surgeons and farmers alike! It also, very importantly, can highlight problems with a drying off routine and educate farmers about the importance of each step in the drying off procedure.
In context, the ‘dead cow’ is dramatic and understandably may be in the farmer's memory forever, but is an uncommon occurance. On many farms selective DCT and the use of internal teat sealants reduces clinical mastitis rates, leading to a reduction in pain, production losses and culling. These benefits may be less obvious to the farmer until farm records are analysed. With every intervention, benefits and risks have to be weighed against each other. In this situation the evidence is clearly in favour of selective, targeted DCT and the use of internal teat sealants.
How could we approach the sceptical farmer?
Different possible strategies are available:
- Emphasise the public pressure — supermarkets, consumers, etc. Point out the global antimicrobial resistance crisis. The Responsible Use of Medicines in Agriculture Alliance (RUMA) target task force sets a target of lower aDCT and higher use of internal teat sealants. This is a common ‘conventional’ approach. Many farmers feel forced to either adapt or leave the industry. However, external pressure is met with resistance by many individuals who feel not in control of their actions. Consequently, changes may not be persist.
- Use peer groups and ‘hidden’ pressure by colleagues: organise ‘stable schools’, ‘field labs’, for farmers to meet on a successful host farm. The veterinary surgeon's role becomes that of a facilitator, a ‘catalyst’, farmers do adopt well from colleagues they trust. A climate of openness and honesty is often generated in these groups, and they have been shown to effect change (Vaarst et al, 2007).
- One to one communication with the farmer, using motivational interviewing. This technique, which was developed in addiction therapy, avoids a confrontational approach and tries to direct a conversation to make the farmer say (and own!) what we previously advised him/her. The technique has been applied to a veterinary context by Bard et al (2017). Many of the points above can be used, emphasising more the benefits to the farmer — using less antibiotics ultimately gives better results to you, and results in fewer mastitis cases and less money wasted. It is important not to put a cost figure for mastitis on the table but try to get this figure from the farmer during a discussion by reminding him/her of all aspects of losses. A figure which is at the lower end but calculated by the farmer (and therefore trusted by the client) is probably more effective to trigger change than a ‘real’ or well researched figure which he/she is just told (and either believes or not).
- It also makes sense to take a step by step approach to start with. Farmers who currently use aDCT without the use of teat sealants could introduce internal teat sealants gradually and monitor progress in the first period. Then antibiotics could be left out (targeted dry cow therapy) initially on a proportion of cows which are at low risk of carrying IMI (e.g. last three somatic cell count readings below 100 000 and no clinical mastitis in the lactation). Again, an introductory training session on the correct use of teat sealants is highly recommended. Hopefully this approach will build confidence and win over the farmer.
- Where farmers struggle to dry off cows hygienically or are pressed for time veterinary practices could also offer an allround service by technicians — selecting the cows to receive antibiotic treatment and providing regular visits to perform the drying off procedure.
Conclusion
Internal teat sealants and selective dry cow therapy DOES:
- Prevent more new IMIs during the dry period than the use of aDCT alone
- Reduce the risk of clinical coliform mastitis post calving
- Reduce the quantity of aDCT used on most dairy farms
- Reduce the likelihood of exposure of newborn calves to antimicrobial residues and potentially resistant bacteria via colostrum.
Internal teat sealants and selective dry cow therapy DOES NOT:
- Significantly reduce the mg/kg population correction unit (PCU) figure of antimicrobial usage — intramammary preparations (dry cow and lactating) only make up 1% of total antimicrobial ingredient sold for livestock in the UK, and dry cow tubes are used at about 1 g per cow per year (VMD, 2018). In order to reduce the mg/kg PCU figure, savings in other areas can achieve higher gains (e.g. injectable antibiotics, footbaths). While a reduction in antimicrobial use is still important for the reasons above, this should be pointed out to the client — if the expectation is great progress at the next antibiotics audit, there may be disappointment depending on how antimicrobial usage is measured. The DCDvet figure is more appropriate to use. (A summary of the current metrics of measuring antibiotic usage is given by Mills et al, 2018)
- Compensate for poor dry cow hygiene — high infection pressure will overcome the protective effect of internal teat sealants.
Communicating these points effectively and starting or continuing the journey with the client is a challenging but potentially rewarding veterinary task.
KEY POINTS
- The cost of mastitis is widely underestimated, with the cost of spread often not accounted for.
- The dry period is the weakest link on many farms.
- Internal teat sealants prevent more new intramammary infections (IMIs) during the dry period than the use of antibiotic dry cow therapy (aDCT) alone.
- Some farmers are resistant against changing long established and ‘proven’ protocols
- A sympathetic approach and motivational interviewing in combination with staff training and ‘stable schools’ can be an effective way to facilitate change.
References
Reducing antibiotic use in dairy herds: selective antibiotic dry cow therapy
The term ‘selective dry cow therapy’ has in recent years become used to describe a decision making process at drying-off whereby low somatic cell count, uninfected cows are not treated with intramammary antibiotic dry cow therapy. While the name suggests that this is a relatively new approach, the concept itself is not new, and was developed from underpinning research in the late 1990s and early 2000s. Variations on the original research have led to herds adopting this approach unsuccessfully, either through poor intramammary infusion technique, a lack of individual cow somatic cell count data or unsuitable thresholds at the cow level. Continued barriers to the adoption of a selective approach to antibiotic dry cow therapy will be discussed in this article, along with strategies that can be adopted by veterinary surgeons to reach those herds that remain unwilling to implement this approach on farm.
The term ‘selective dry cow therapy’ began appearing in the literature nearly 10 years ago as studies took the underpinning research that described the use of internal teat sealants in uninfected cows and produced data on outcomes in the next lactation (Rajala-Schultz et al, 2011), or attempted to refine the process of ‘selection’ of those cows that may require antibiotic dry cow therapy using other methods such as bacteriology (Cameron et al, 2014). Underpinning research, however, takes us as far back as the late 1990s, where the importance of dry period infections in mastitis control were highlighted in ground-breaking UK work (Bradley and Green, 2000), and followed shortly by a study that showed antibiotic dry cow therapy decisions taken at drying-off affected the rate of clinical mastitis in the next lactation (Bradley and Green, 2001a). Original research with the internal teat sealant OrbeSeal® (Zoetis) quickly followed, and clearly showed that low somatic cell count cows treated at drying-off with internal teat sealant alone acquired significantly fewer infections with Escherichia coli, and all coliforms combined, when compared with cows that received an antibiotic dry cow therapy product (Huxley et al, 2002). This team went on to publish a pair of clinical articles that attempted to bring all this research together, present a practical approach to the practitioner and talk about the ‘prescription’ of dry cow therapy via a rational approach to decision making on farm (Green et al, 2002; Bradley et al, 2003).
Processors and dairies began adopting the term selective dry cow therapy as requirements for herds supplying milk under certain contracts were outlined, for example Arlagaarden UK in 2015. Following the publication of the O'Neill report and the Government's response to this document (HM Government, 2016), the use of antibiotics to prevent disease in livestock is under increased scrutiny, and sector specific approaches set out in the livestock industry. For the dairy sector, a blanket approach to antibiotic dry cow therapy is a very good example of what is termed ‘unnecessary’ or ‘inappropriate’ use of antibiotic, and the Responsible Use of Medicines in Agriculture Alliance (RUMA) Targets Task Force proposed a 20% reduction in the use of antibiotic dry cow therapy to be adopted by 2020 (RUMA, 2017).
Despite the original work around the use of teat sealants alone in low somatic cell count cows at drying-off, and all the research work that has followed after, there continue to be barriers to the adoption of a selective approach. A quick search using the PubMed database finds 68 published papers on the subject of selective dry cow therapy (https://www.ncbi.nlm.nih.gov/pubmed/?term=selective+dry+cow+therapy) and the dissemination of the science clearly remains an important consideration for tomorrow's, as well as today's veterinary advisors. However, it is perhaps the ‘softer’ skills that we sometimes needs to focus on with our clients — a survey of farmers in the Netherlands reported several factors that were associated with the probability of applying a selective approach to antibiotic dry cow therapy, including usage of internal teat sealants and uncertainty about whether or not cows would recover in the absence of antibiotic (Scherpenzeel et al, 2016). This article attempts to provide some take home messages as veterinary advisors tackle frequently asked questions from their dairy clients on this topic, and is particularly aimed at veterinary surgeons who are trying to achieve a mind-set change with their clients. The article is divided into two sections — examples of those barriers that reflect farmers that have no intention to change, and examples of those barriers that are put in place by clients who realise this approach is the ‘right thing to do’ but perceive obstacles or difficulties along the way. It is important that we do not forget the benefits of the use of antibiotic dry cow therapy — but instead focus on the need to target antibiotic dry cow therapy at those cows that are likely to benefit the most.
No intention to implement a change to selective antibiotic dry cow therapy
‘If I take a selective approach to antibiotic dry cow therapy my cell counts go up’
For many herds, the barrier to the adoption of a selective approach is simply one of ‘why do I need to’, as many herds report that the bulk milk somatic cell count is low and a blanket approach to dry cow antibiotic is therefore ‘working’. The approach in these herds is therefore one of understanding that this is a great example of the client needing to move from ‘no intention’ to ‘wanting to change’ (Higgins et al, 2012). The arguments could therefore include getting the client to think about what effect antibiotic dry cow therapy may be having in the low somatic cell count cows, i.e. those below 200 000 cells/ml where the likelihood of a major pathogen infection at drying-off is low (of which there are a great many in these low cell count herds), as well as those methods that challenge the social ‘norm’. The former can be usefully discussed in the light of published UK work where the infusion of antibiotic dry cow therapy was associated with an increased risk of clinical coliform mastitis in the next lactation (Bradley et al, 2010), particularly when these herds begin to think about clinical mastitis rather than cell count outcomes. Coliform mastitis conjures up the picture of the toxic, dying cow, but we must remember that the majority of coliform infections often do not present with severe clinical signs, and recurrence of clinical mastitis can be a feature of infection (Bradley and Green, 2001b).
Challenging the social norm is usefully done by inviting discussion groups to herds that already take this approach, particularly when the invitation is around another topic altogether and preferably one of interest to the client we are trying to influence. These herds are unable to appreciate that they are increasingly in the minority, so discussing articles from the media are also useful here — particularly when articles are about herds that are well known in the area and to the client in question.
‘We can't use internal teat sealants on their own — we might kill the cow’
This remains a huge challenge and is often the greatest barrier to the implementation of a selective approach to antibiotic dry cow therapy. Despite many published papers describing cows infused with internal teat sealant alone, nothing short of demonstrating infusion technique with reluctant clients and proving that cows can be dried off safely will often do here. Visits to neighbouring herds that implement a selective approach often help, particularly when these more progressive clients are happy for you to demonstrate infusion technique on their cows. As veterinary surgeons at undergraduate level we are not often taught or shown correct intramammary infusion technique and to this end, AHDB Dairy have produced several resources in this area designed to help clients and veterinary surgeons alike (https://youtu.be/gJH-v177D1xc; http://dairy.ahdb.org.uk/dry-cow-management). To avoid putting clients on the spot, this author often finds it helpful to use the exercise to be seen to be teaching undergraduate veterinary students rather than the client directly, although this requires close supervision (Figure 1). Often, the existing approach to intramammary infusion is inappropriate, and we need to stress aseptic technique and demonstrate it. The inclusion of a pre-milking teat disinfectant is often lacking, as is clean cotton wool and surgical spirit, the storage of which can be poor. Only by demonstrating can we itemise the steps involved in aseptic infusion of internal teat sealant and avoid generic statements such as ‘it's all about attention to detail’.

‘Our dry cow environment isn't good enough so we have to use antibiotic in all cows at drying-off’
The third barrier to even the consideration of adoption of selective dry cow therapy is in some ways the hardest, as ultimately we know from research that the successful reduction of dry period infections comes from excellent management of the dry cow environment (Green et al, 2007). The perception that antibiotic dry cow therapy is required when dry cows are housed (particularly on loose yards) is a common one, and the concern is raised that the environment is not good enough to allow for internal teat sealant alone. It is interesting in these herds to challenge this position by looking at the records and data, and turning that on its head. For example, the perception that the new infection rate during the dry period as measured by cell count is low because all cows receive antibiotic can be readily refuted when the client is shown that the dry period new infection rate averages 20% despite blanket use of antibiotic dry cow — provided individual somatic cell count data exist of course.
Other interesting points of discussion are to ask the client if they believe that just because the dry cow antibiotic ‘lasts a long time’ that this is the same as remaining above a level that removes bacteria — the difference between maximum residue limit (MRL) and minimum inhibitory concentration (MIC). Of course this does not address the dry cow environment itself — but here again, we may take advantage of resources that are readily available to assist with the discussion and provide a starting point (https://dairy.ahdb.org.uk/media/1669377/AHDB_DryCowManagement_WEB_2018-01-18%20(1).pdf). Great examples are spring block calving herds where a meeting scheduled before drying-off begins can have great benefits; the client can ‘walk’ through from drying off to calving – where the cows will go, where they will be housed, how long for and at what stocking rate etc — and try and come up with ideas on how to reduce infection pressure.
Intention to implement a change to a selective approach is present — ‘wanting’ to be ‘doing’
‘How do I know which cows are infected in my herd?’
Perhaps more technical questions come from those clients wishing to adopt a move to a selective approach to drying-off but are unsure about methods to detect which cows are likely to be infected. These broadly fall into three areas: cow-side tests such as the California Mastitis Test (CMT), bacteriology at drying-off using on-farm culture and the use of individual somatic cell count. For those clients with the latter, it is a reminder that the original research around the use of internal teat sealants was done using a threshold of 200 000 cells/ml and was then refined to focus on the last THREE recordings in lactation prior to the drying-off event. A lack of individual somatic cell count data is in itself a barrier to the adoption of selective dry cow therapy — but with some flexibility this can be overcome. A good example is block calving herds where infrequent milk recording can be an issue unless conversations are had about ‘clustering’ recordings at the back end of lactation and shortly after calving to enable drying-off decisions to be made.
As further research is published around the use of on-farm culture, the application of a bacteriological outcome as well as somatic cell count is often put forward as a method to differentiate infected and uninfected cows with a greater degree of accuracy. However, research from North America showed that only 1.2% of quarters and 0.5% of quarters were found to be infected with an environmental Streptococcus spp. and Staphylococcus aureus respectively when samples were submitted from cows that were below a threshold of 200 000 cells/ml in the last three milk recordings prior to drying-off, and that had not been reported with clinical mastitis in the last 3 months prior to drying off (Cameron et al, 2013). It is perhaps more important to challenge the concept of a false-positive diagnosis with bacteriology — in other words, just because we have cultured a Gram-positive organism at drying-off, is this a requirement for antibiotic dry cow therapy? A coagulasenegative Staphylococcus spp. can be readily recovered from low somatic cell count cows at drying-off, but this does not mean this cow is infected and requires treatment. The use of on-farm culture to inform decision making at drying-off is often put forward as a ‘Gold Standard’ test, but will also have inherent issues with sensitivity and specificity — and on-farm culture performed poorly is likely to be worse than using cell count data.
On its own, the California Mastitis Test is unlikely to be sufficient as a test at drying-off, as there are issues with both test sensitivity (the impact of missing an infected cow) and particularly test specificity, with the latter interesting to point out to clients given the likelihood of treating an uninfected cow with antibiotic, particularly in low cell count herds.
‘What about missing some infected cows?’
Clients are rightly concerned about missing some cows which are likely to be infected with a major pathogen and the impact that they may have on herd mastitis epidemiology. Improvement in test sensitivity at drying-off when using cell count data can be achieved by lowering the threshold in herds where the prevalence of infection is high — for example using a threshold of 150 000 cells/ml or even 100 000 cells/ml in higher cell count herds. Note that there is no benefit to lowering the threshold in low prevalence herds! Clearly, the monitoring of outcomes then becomes important to ensure cure rates during the dry period are achieving what we expect — and that the apparent cure rate is not impacted by a high rate of re-infection from the dry cow environment. In herds with a low prevalence, concerns about missing infected cows are often unfounded when we look at cell count dynamics in the herd that describe risk of infection during lactation. Cows infected with a major pathogen in these low cell count herds may be a source of new infection — but using data analysis, and reassuring the client that the current new infection rate during lactation has averaged 5% in the last year, often helps to allay any fears.
‘Some of our staff are unable to carry out this task’
Often overlooked are the practicalities of implementing changes on farm — the team are motivated, the client wants to make the change, the technical aspects are worked out, but remembering to do it, as well as ensuring staff are trained and have the time to carry out the task, are essential. At other times we are dealing with a diplomatic situation where the member of staff who dries off 90% of the herd is incapable of carrying-out the task correctly and we need to find ways of re-distributing the workload such that a different member of the team can dry the cows off. It may be that drying-off now occurs on a different day, allowing for more time or the production of an action list. Again, the veterinary advisor is in an ideal position to appreciate the nuances of the day to day farm routine.
Conclusions
Appreciating exactly what the barriers to the adoption of a selective approach to antibiotic dry cow therapy are allows the veterinary advisor to better understand the arguments they have to make in order to facilitate change on farm. There is little or no point discussing diagnostic tests or somatic cell count threshold when fundamentally entrenched positions such as the use of internal teat sealant or the dry cow environment need to be confronted. Some herds will never change, but many others herds will, either because they have to or because the social norm becomes challenged and this is where the role of the veterinary advisor is key to helping our clients implement the necessary changes they need to make this happen, from staff training to improved environment management.
Finally, it must be remembered that monitoring of these data are paramount to provide positive reinforcement, and that this data is targeted to the dry period. An increase in bulk milk somatic cell count or clinical mastitis rate during the summer that is then immediately blamed on selective dry cow therapy in the absence of appropriate data analysis is a good example — the dry period new infection rate may be unchanged but the rate of new infection in the low yielding group at grass may have significantly increased — clearly nothing to do with the change the client was concerned with. Close monitoring of new infection and cure rates allows for positive feedback to the team as well as tweaking of management to ensure a successful implementation, and should always be provided.
KEY POINTS
- Underpinning research work from the late 1990s and early 2000s introduced the concepts of dry period infections from the environment, the benefits of an individual cow approach at drying-off and the importance of internal teat sealant alone in low cell count, uninfected cows at drying-off.
- The adoption of selective dry cow therapy as it has become known is increasingly seen as an excellent example of reducing ‘inappropriate’ use of antibiotic in dairy herds.
- Barriers to the adoption of selective dry cow therapy in herds fall into those where the farmer has no intention to change and those that highlight a willingness to adopt the change but some apprehension around implementation.
- For those farmers with no intention to change, discussions will often centre around the use of teat sealants in general, visits to other clients and the challenging of social norms.
- For those farmers wishing to move from ‘wanting’ to ‘doing’, they may require reassurance with more technical aspects such as thresholds or tests, as well as help with practical day to day implementation.

