During August a 5-year-old Holstein cow, which calved 2 weeks previously, is presented with respiratory distress with occasional open-mouth breathing. The milking herd is managed indoors year-round but the dry cows have access to pasture. The cow had been treated with oxytetracycline and meloxicam for 3 days before veterinary examination. The cow has not been observed eating today. Milk yield is reported to be 12–15 litres per day for the past week (expected to be 45 litres per day at peak). On inspection, the cow's neck is outstretched with the head held lowered and the ears directed caudally with a painful expression (Figure 1, Video 1). The cow has a low body condition score (BCS 1.5); the abdomen is drawn-up with an obvious sunken triangle behind the rib cage caused by poor rumen fill. The coat is long and lacks its normal sheen. There is a purulent nasal discharge. The rectal temperature is 39.0°C. The respiratory rate is 32 breaths per minute with an expiratory grunt. There is obvious halitosis and occasional coughing. Auscultation reveals no adventitious lung sounds only muffled heart lung sounds. There is no peripheral oedema and no jugular pulse. The cow is not lame and there are no joint swellings. There is no vaginal discharge and no history of retained fetal membranes nor mastitis. There are no other cattle affected at present although several cows have been observed with similar, but less severe, signs over the past 12 months. There has been no history of infectious bovine rhinotracheitis (IBR) in the herd from bulk milk testing.

Cattle self assesment: QUESTIONS
- Which conditions would you consider in a differential diagnosis list?
- What further examinations would you undertake?
- What is the prognosis for this cow?
- What is the likely best treatment strategy?
Self assesment: ANSWERS
- Conditions to consider and order of most likely causes:
- Recrudescence of chronic pneumonia (bronchiectasis)
- Lungworm
- Infectious bovine rhinotracheitis
- Hepatocaval thrombosis
- Endocarditis
- Traumatic pericarditis
- Cardiac tumour (heart base tumour)
- Recrudescence of chronic pneumonia (bronchiectasis) is the most likely explanation of the clinical signs noting that oxytetracycline is not the best choice of antibiotic and meloxicam is unlikely to affect outcome
- Lungworm must be excluded noting that this cow had been at pasture albeit 2 weeks previously. A Baermann test can be undertaken overnight in the practice laboratory, however, note the 3 week prepatent period and the possibility of re-infection syndrome giving a negative result. No other cattle are affected and there is only occasional coughing
- Infectious bovine rhinotracheitis should be considered but ocular involvement may be expected and there is usually marked pyrexia (>40.5°C). No other cattle are affected (yet)
- Endocarditis is often present without producing a heart murmur although joint effusions (hock and fetlock joints) are common
- Hepatocaval thrombosis would produce epistaxis although large volumes of blood can be swallowed
- Cardiac tumours (heart base tumour) are rare and associated with considerable pleural and pericardial effusions causing muffled heart sounds. Signs of right-sided heart failure are usually present.
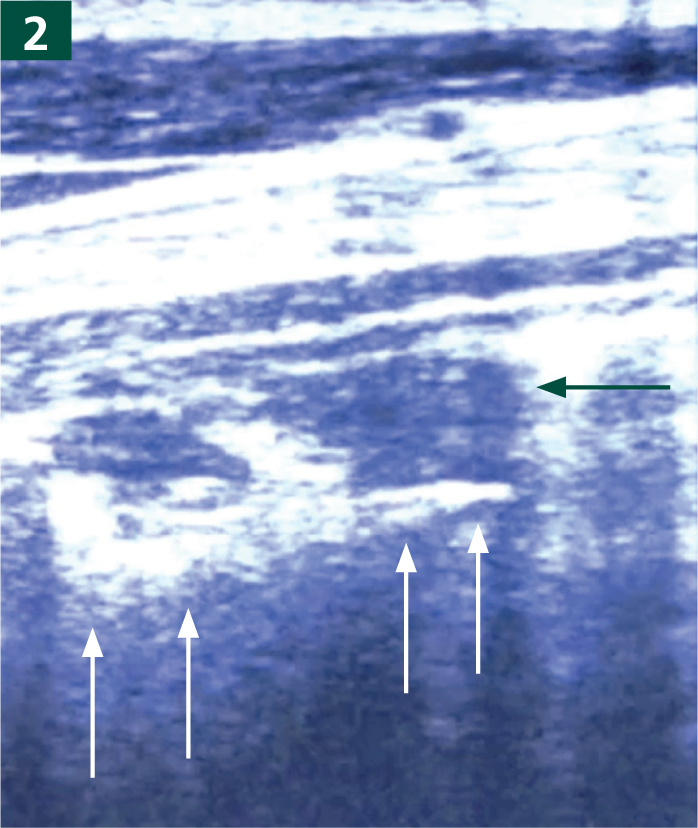
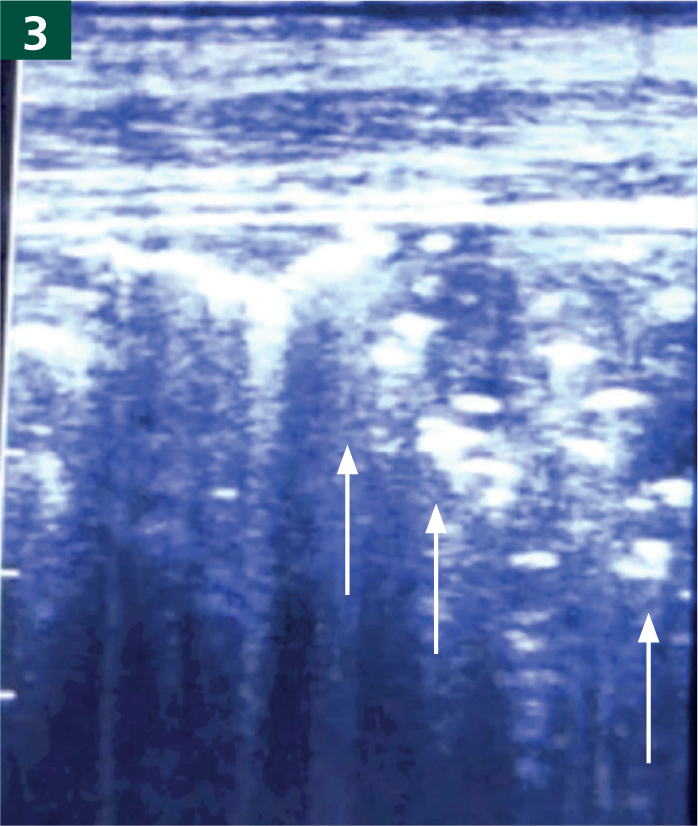
- Ultrasonography using a 5 MHz linear (rectal) scanner. The sonograms are presented with the probe head/chest wall at the top of the image, dorsal is to the left and ventral to the right of the image. Centimetre markers are displayed on the margin of the right image for both figures (Figures 2 and 3).
- The extent of lung consolidation/pathology (Figure 4) can be determined by measuring its dorsal margin vertically from the point of the elbow and adding the values from both sides of the chest. The prognosis is poor when this value exceeds 40 cm (600 kg cow). The value in this cow was 31 cm.
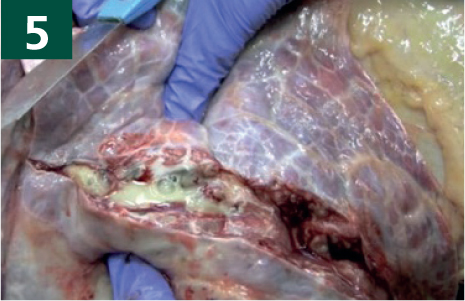
- Bronchiectasis is the term given to permanently-dilated small bronchi and bronchioles located in the ventral parts of the lungs which contain a wide range of microorganisms, predominantly Trueperella pyogenes, causing chronic disease (Figure 5). T. pyogenes is a species of non-motile, facultatively anaerobic, Gram-positive bacteria and is fully susceptible to procaine penicillin. The action of procaine penicillin is time-dependent, therefore an extended course of treatment is necessary (daily treatment for 3 weeks). There is no indication to use penicillin/streptomycin combination nor ampicillin/clavulanic acid combination. Long-acting penicillin injected every third day does not work. A single injection of dexa-methasone was administered to alleviate pulmonary oedema associated with the bronchiectasis. Pulmonary oedema was not proven but may explain the severity of clinical presentation when lung consolidation measured 31 cms. The cow is shown 1 week after commencing penicillin treatment (Figure 6, Video 3). The cow's future in the herd is likely to be determined by future milk yield and the interval to conception after such a severe illness, albeit exacerbated by delayed treatment with the correct antibiotic.